A promising new treatment for PTSD

Idit Negrin will try anything to overcome the trauma that has been with her since she attended the Nova Music Festival on October 7, when Hamas killed hundreds of civilianss. “We saw the terrorists, they started shooting at us,” he said. He ran for his life.
After that, “I woke up every night, every night at 3 o’clock screaming and sweating and shaking. I think a day, or two days after that, I felt like I was falling, crying.”
We caught up with her this summer as she is in the second third of her 60-session hyperbaric oxygen therapy (HBOT) course. A drug that has long been used to combat divers’ stress syndrome, and wounds that will not heal. But at the Sagol Center for Hyperbaric Medicine and Research, in Be’er Ya’akov, Israel, they are now treating a very different disease: post-traumatic stress disorder, or PTSD.
Negrin described his experience with PTSD: “You feel like you’re going crazy. I’m calling people and yelling, ‘There’s another terrorist attack!’ Then you understand that you can’t control your brain.”
Negrin is trying to regain that control, along with about 650 other survivors of the 7th of October suffering from PTSD who are treated, for free, and military veterans at the Sagol Center – currently the largest center in the world.
CBS News
Dr. Shai Efrati runs this clinic, where they treat up to 350 patients a day, and are at the forefront of this type of medicine. “What we are actually doing is manipulating the body,” said Efrati. “Hypoxia, a lack of oxygen, is a powerful stimulus to induce the entire repair process to reverse.”
Efrati says they’re making adjustments to the body and brain inside these pressurized chambers, where it feels like you’re diving down to 30 feet. Patients breathe pure oxygen, which under such high pressure conditions the body can absorb up to 16 times the normal level. After that, the mask is removed for five minutes.
Efrati said, “The drop from very high to normal is translated to the same level as hypoxia, as a lack of oxygen. That causes the body to initiate stem cells, and for the first time even in humans, we can see. the generation of new neurons, the generation of blood vessels new blood vessels in the brain And this is thought-provoking.
The treatment has been described as “not approved” and “not proven.” “When we talk about hyperbaric oxygen therapy, this is what it should look like,” Efrati said.
“You say there are many crooks out there?” Doane asked.
“Of course. And this is not only good, it can even be dangerous.”
CBS News
Dr. Efrati is always trying new ways to use this treatment. In his clinic near Tel Aviv, we saw how they give hyperbaric medicine to athletes (“If we can reduce the recovery time, you can push harder to do exercises”), and help patients with brain injuries to move again by using the growth of new neurons and blood vessels in the brain.
“It’s not like we’re fixing his running,” Efrati said of a particular athlete. “We’re fixing the brain.”
They have published several studies, looking at PTSD in veterans. One, out today, found that 68% of patients showed significant improvement. One reported that PTSD relief lasted at least two years, longer than other established treatments. “We want to evaluate everything properly,” said Efrati.
It’s perfect enough that the Israel Defense Forces, or IDF, asked Efrati’s team to stop testing and start treating. The doctor says that while you can always ask for more data, “You see the evidence in front of you.”
Shachar Mizrhai was one of those IDF veterans mentioned in 2018 in the first clinical trial. He was a soldier during Israel’s 2014 attack on Gaza and was in an armored vehicle when it was attacked. For a short time, he thought about survival; suffering came later. “I can’t sleep at night,” he said. “When I put [on] uniform, I feel like I want to die. I smell blood. I smell war.”
He has tried drugs, therapy and sleeping pills. He was thinking of killing himself. “Nothing has helped me get back to health,” he said. “And I heard that this might be useful, and maybe this is my last chance before I end my life.”
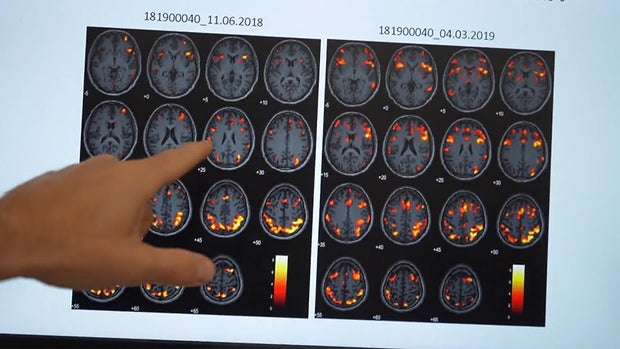
Dr. Keren Doenyas-Barak, head of the PTSD program at the Sagol Center, followed Mizrhai through his 60 sessions, and showed us his brain scans from June 2018, and March 2019, highlighting the activation of areas used to effectively control emotions, or process . information. The brain scan images later were brilliant; that was not possible before treatment.
CBS News
“A lot of people tend to think of PTSD as a psychological thing, not a biological thing,” Doenyas-Barak said. “So, we treat PTSD very similarly to other brain conditions.”
For Mizrhai, the treatment changed everything:” “It was the first time I could hear again. When I started sleeping at night, I wasn’t so scared. It makes me feel alive again. … I was a dying man, and after this, I am a living man.”
North Carolina Republican Congressman and medical doctor Greg Murphy said, “If it’s given in Israel and they get such good results, why don’t we give it to the United States?”
That’s the question Murphy — a member of the House Committee on Veterans Affairs — is raising in the halls of Congress. One in ten of its members are veterans. “I love our VA,” he said. “But we don’t reach a certain level for our veterans when they are killing 22 people every day. And if we do something and there is a treatment that has shown positive results, I believe that is medical malpractice for our veterans.”
In 2023, he introduced the National Traumatic Injury Treatment Act. “Basically we want the VA to do a pilot study within their boundaries to see if they can demonstrate that hyperbaric oxygen works or not,” he said.
And what does he hear from the VA? “They don’t want to do anything, they just raise their hands,” he said. “The reasons we’ve heard are, ‘Well, the results have been mixed.’ Great. Look at the results over the last 15 years.
The Sunday Morning newspaper requested an interview with the Department of Veterans Affairs, but it declined to comment.
In Salt Lake City, Utah, we met Dr. Lin Weaver, director of Hyperbaric Medicine at Intermountain Health. They treat about 20 patients a day, which clearly puts the large numbers – 350 every day – treated in Israel. He says that they use their hyperbaric chambers for PTSD patients rarely, because it is expensive, but he has seen good results: “I have had patients that I have treated. Everyone has improved amazingly,” said Weaver.
But insurance companies say there isn’t enough evidence for PTSD to work. And in the US, out-of-pocket costs rise above $50,000.
“What’s required is like a drug test,” Weaver said. “But these trials take years to accomplish. It all depends on, ‘Is there action? And is there a source of money?’
Doane asked, “But if doctors like you feel so strongly that this works, why isn’t there enough pressure from people like you to say, ‘Prove this’?”
“Well, believe me, we tried,” Weaver replied. “I have submitted proposals to after-school funding agencies. So far, they have not accepted.”
Doane asked Dr. Efrat, “You’re outside the border here of medicine. Is there any danger in that?”
“As a scientist, I will always tell you that I need more research, I need more data,” he replied. “But doctor, if I sit in front of you and look you in the eye, you have a problem now. This is our job as doctors.”
Idit Negrin says that this treatment gives her hope that she can overcome that nightmare at the Nova Music Festival. He hopes that with treatment, he can get on with his life.
But she wears a reminder — a Nova necklace — while she’s receiving treatment. “I’m not taking it off my neck,” he said.
His progress motivates Dr. Efrat to continue to innovate, thinking about the future so that his patients can process the past.
Doane said, “Some people will listen to this and say it sounds too good to be true.”
“Yes, I know,” said Negrin. “But it’s true.”
CBS News
For more information:
Story produced by Sari Aviv. Editor: Ed Givnish.
See also:
Source link